Predicting Spinal Screw Loosening using Automated Biomechanical Simulations
Beyond Traditional Bone Density: A Smarter Way to Predict Surgical Complications
When surgeons perform spinal fusion surgery, they secure pedicle screws into the vertebrae to stabilize the spine. While this procedure helps millions of patients each year, one concerning complication is screw loosening. This can lead to persistent pain, failed fusion, and the need for additional surgery.
Traditionally, doctors have relied on CT scans to measure bone density (using Hounsfield Units) to predict which screws might loosen. The logic is straightforward: denser, stronger bone should hold screws better. We have developed a more sophisticated approach that considers not just bone quality, but also the forces acting on each screw.
A Comprehensive Biomechanical Model
Our approach combines multiple types of data and advanced computer simulation to predict screw loosening risk. Starting with a patient's preoperative CT scan and surgical plan, our automated pipeline:
1. Analyzes Patient-Specific Anatomy and Forces
The model first examines the CT images to understand the patient's unique spinal geometry, alignment, and curvature. Using musculoskeletal modeling, it then calculates the personalized forces acting on each person's spine based on their body weight, posture, and the specific configuration of their planned fusion construct – rather than assuming all patients experience identical loads.
2. Maps Detailed Bone Properties
The system converts CT measurements into a detailed map of mechanical strength throughout each vertebra, understanding the exact material properties surrounding each planned screw location.
3. Simulates Screw Loading with Finite Element Analysis
The model simulates how forces distribute through the bone surrounding each screw. This advanced computer simulation predicts stress concentrations around each planned screw location.
4. Generates Risk Assessment
The system calculates a "loading factor" that represents how close the bone is to its failure point during normal activities like standing. This biomechanical metric is then compared against our validated clinical outcomes database to generate a patient-specific risk score for screw loosening, translating the engineering analysis into clinically meaningful predictions.
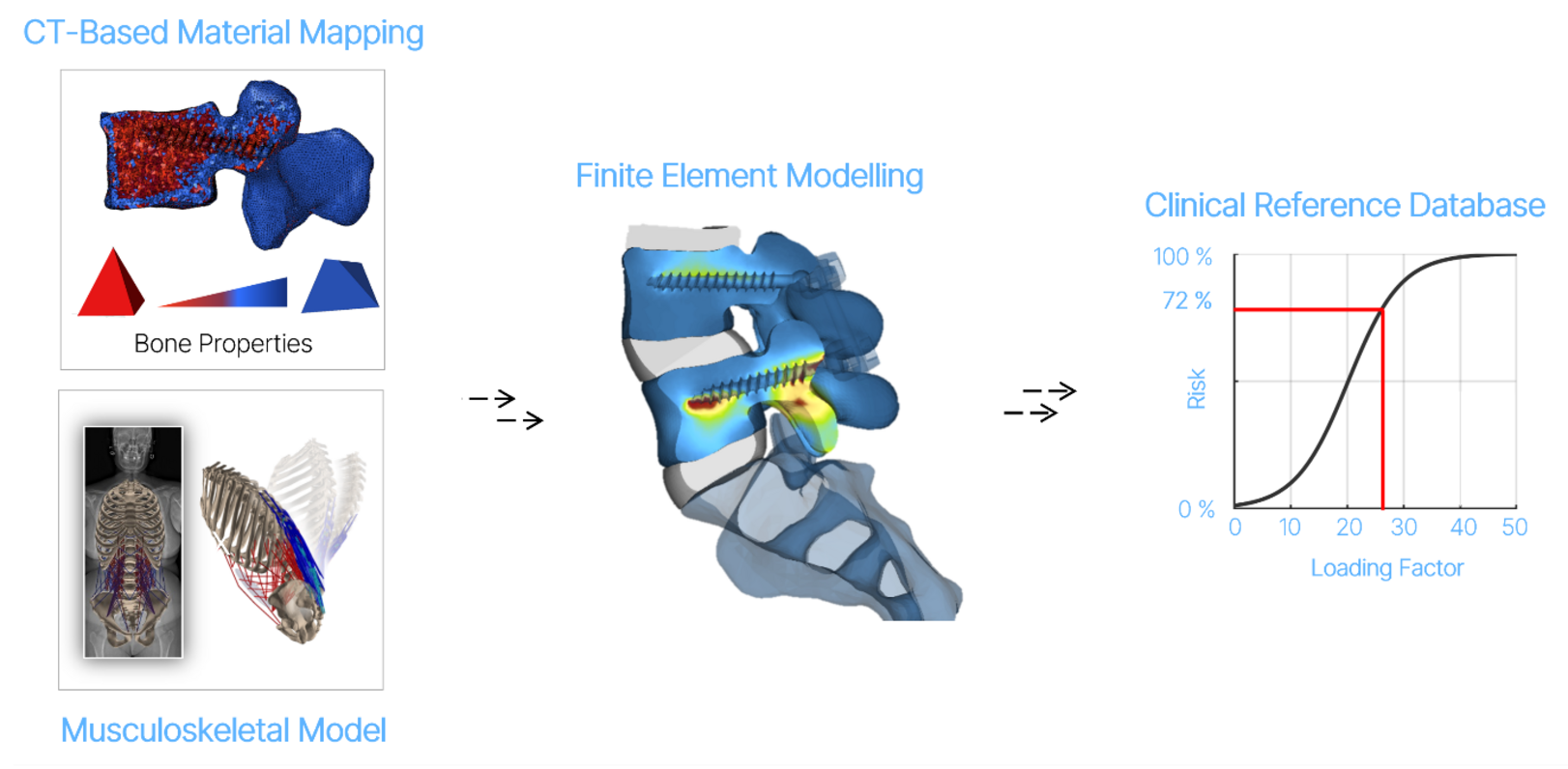
Figure 1: Workflow of the developed modelling pipeline.
Clinical Advantages
This biomechanical approach offers several key benefits over traditional bone density measurements:
- More comprehensive assessment: Instead of just measuring bone quality, the model considers both bone strength and the actual forces each screw must withstand.
- Patient-specific predictions: Each analysis is tailored to the individual's anatomy, body weight, and planned surgical construct.
- Automated and efficient: The entire analysis runs automatically in minutes, making it practical for clinical use.
- Actionable insights: By providing detailed risk assessments before surgery, the model can help surgeons optimize screw placement and dimensions, identify cases requiring bone cement augmentation, and ultimately reduce screw loosening complications while improving long-term outcomes.
Proof-of-concept Planning Solution
To demonstrate the clinical potential of our biomechanical modeling approach, we developed a web-based prototype that integrates directly with the patient-specific simulation framework. This proof-of-concept planning tool allows surgeons to upload CT scans, create surgical plans and automatically generate personalized risk assessments for each planned screw location. The interface visualizes bone density distributions, predicted stress distributions, and risk scores in an intuitive format that supports clinical decision-making. The interactive planning tool is accessible at:
https://app.spineplanner.com/login
(demonstration version - not for clinical use)



