Research Projects
The Spine Biomechanics group comprising engineers from ETH Zurich and surgeons from the Balgrist University Hospital. Together they conduct translational research at the interface between fundamental biomechanical research and the development of clinically applicable methods. The interdisciplinary approach guarantees a high level of expertise required to address relevant clinical issues. The group has established a fully equipped spine lab with custom test setups for biomechanical in-vitro experiments that is on par with the worldwide leading biomechanical spine laboratories. This equipment has been used for a multitude of biomechanical studies on human spine cadavers to investigate and characterize human anatomy and tissue properties. The obtained results and insights are translated into patient-specific, biomechanical models that are used to optimize pre-operative surgical planning.
Patient-Specific FE Modeling in Spine Surgery
The focus of this project lies on the improvement of spinal surgery outcome through finite element-based functional analysis and surgical planning.
This project is part of the University Medicine Zurich flagship project SURGENT (Surgeon Enhancing Technologies), which was born as a collaboration program between different medical and technical research institutions in Zurich. The overall goal of this collaboration is to use and develop state-of-the-art technologies to improve clinical outcomes and patient safety by enhancing surgical accuracy. The project focus lies in spine surgery and neurosurgery.
During the last decades, computer modelling approaches were established as tools for a more detailed understanding of the intricated mechanisms occurring in the healthy and the pathological spine. Finite element (FE) models allow to compute structural loads in biological tissues (e.g. bones, intervertebral discs, nerves) and devices interacting therewith (e.g. pedicle screws, fusion rods, intervertebral cages). In this project, we aim at using such models to perform functional analysis of specific interventions and to rate the possible treatment options through a quantitative evaluation of the results obtained with varying surgical parameters (e.g. screw position, longitudinal rod position/curvature, strategy for nerve decompression). With automated and efficient biomechanical simulations making use of individualized but low-complexity models, we aim at delivering relevant, quantitative information to surgeons in order to allow them to reduce operating time and increase accuracy during the realization of the surgical plan.
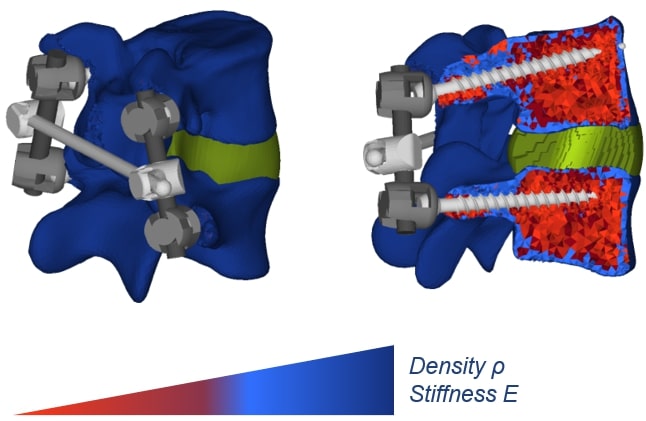
Figure 1: Finite element model of an instrumented lumbar spine segment. Patient-specific information is incorporated in terms of geometry, alignment, and material properties.
For a broad application of such a clinical workflow, the model creation needs to be subject-specific and (semi)automatic, since individually modelling a large number of spines by hand would be a tedious and overall unworkable approach. As a starting point, we use anatomical models derived from segmented lumbar vertebrae of computed tomography (CT) images on which a vertebra-specific statistical shape model (SSM) is fitted [1]. The correspondence properties of these meshes allow us to consistently define muscle and ligament attachment points, boundary conditions, facet joint surfaces, etc. for different vertebral anatomies. Further, the tissue properties can also be obtained from images of clinical resolution (Figure 1).
Figure 2: Von Mises stress distribution in vertebral bone during pedicle screw pull-out simulation.
Implementing an automated pipeline for individualized biomechanical modelling can help to study a great variety of clinical questions. For example, an issue worth addressing is the failure of surgeries because of non-optimal tissue-implant interactions. Spondylodesis is a well-established surgical intervention that aims at improving the conditions of patients affected by a variety of different spinal pathologies. This type of surgery involves the permanent fusion of one or more functional spine units. A common complication associated with these surgeries is screw loosening. We developed and validated an FE pull-out model that is supposed to evaluate patient-specific screw fixation strength by incorporating vertebra-specific bone density distribution obtained from lumbar spine CT scans (Figure 2). The primary output variable is the force required to extract the screw from the bone, indicating failure at the screw-bone interface [2]. The model was used for a first assessment of a multi-objective genetic algorithm which aims at finding the optimal screw position by maximizing the bone mechanical properties in its vicinity (Caprara et al., under review). Modelling axial screw pull-out or caudo-cranial loading of the fusion instrumentation can also help to determine the main load mechanism causing screw loosening. For this purpose, we can make use of retrospective patient data and compare simulated results between cohorts with and without screw loosening in the lumbar spine.
References
- Caprara, S., Carrillo, F., Snedeker, J.G., Farshad, M., Senteler, M., 2021. Automated Pipeline to Generate Anatomically Accurate Patient-Specific Biomechanical Models of Healthy and Pathological FSUs. Front. Bioeng. Biotechnol. 9.
- Widmer, J., Fasser, M.-R., Croci, E., Spirig, J., Snedeker, J.G., Farshad, M., 2020. Individualized prediction of pedicle screw fixation strength with a finite element model. Computer Methods in Biomechanics and Biomedical Engineering 23, 155–167.




